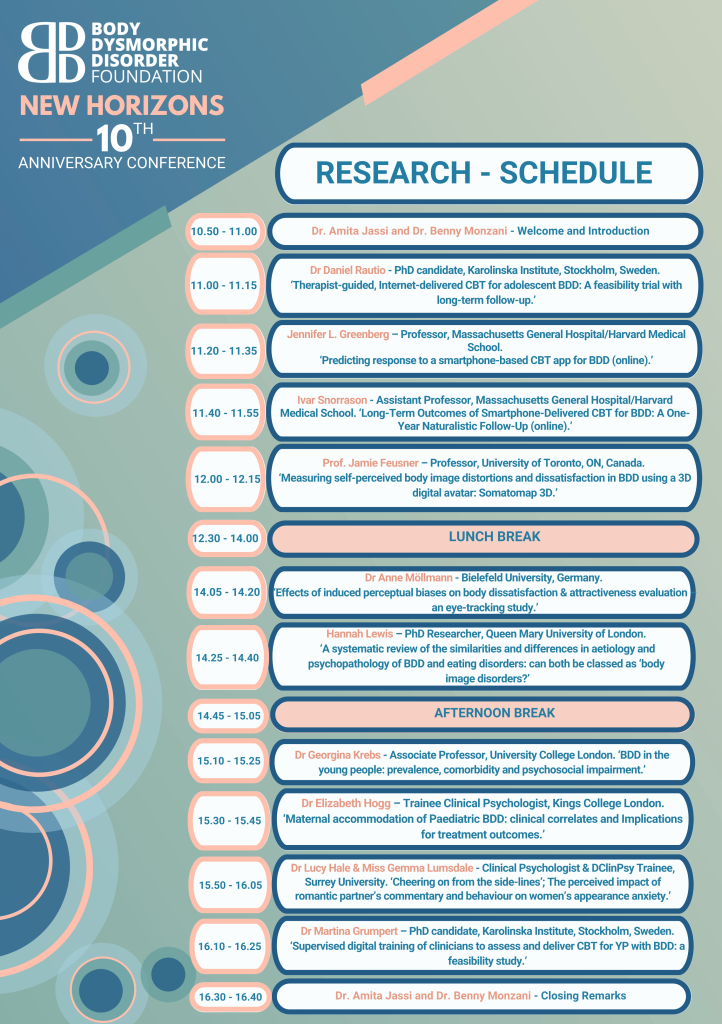
‘Cheering on from the side-lines: the perceived impact of romantic partner’s commentary and behaviour on women’s appearance anxiety’ with Dr Gemma Lumsdale, DClinPsy Trainee, Surrey University.
More stories from the community



























Big thank you to these brave individuals who recently contributed to the LAD Bible Roundtable, sharing their personal stories of BDD. Your courage to use your voices contribute to breaking down stigma around BDD and improving understanding.
The varied perspectives and stories from this discussion are an important reminder that everyone’s BDD journey and recovery will look completely different, and that’s ok.
The discussion covers some really interesting topics, including symptoms, diagnoses, treatment, gender differences, cosmetic surgery, faith, community, rock bottom and turning points in recovery.
Check out the full video below
We will be taking the opportunity to reflect on how far we have come and recent achievements, whilst also looking ahead to advance the future of the charity.
Our conferences are an opportunity to bring together our wonderful BDD community in a supportive, inspiring and informative space. Individuals with BDD, their loved ones, as well as mental health professionals and students come together to learn about the condition, innovative approaches to treatment and hear inspiring stories from those in recovery.
There will be countless opportunities to hear from experts, and learn about varied perspectives in the development and treatment of BDD. The conference is also a space for those living with BDD to find comfort in shared experience, know they are not alone and meet other people in the BDD community. This year, we are introducing a community and support room where those with BDD can connect with others and speak with volunteers about ways to access support through their journey of recovery.
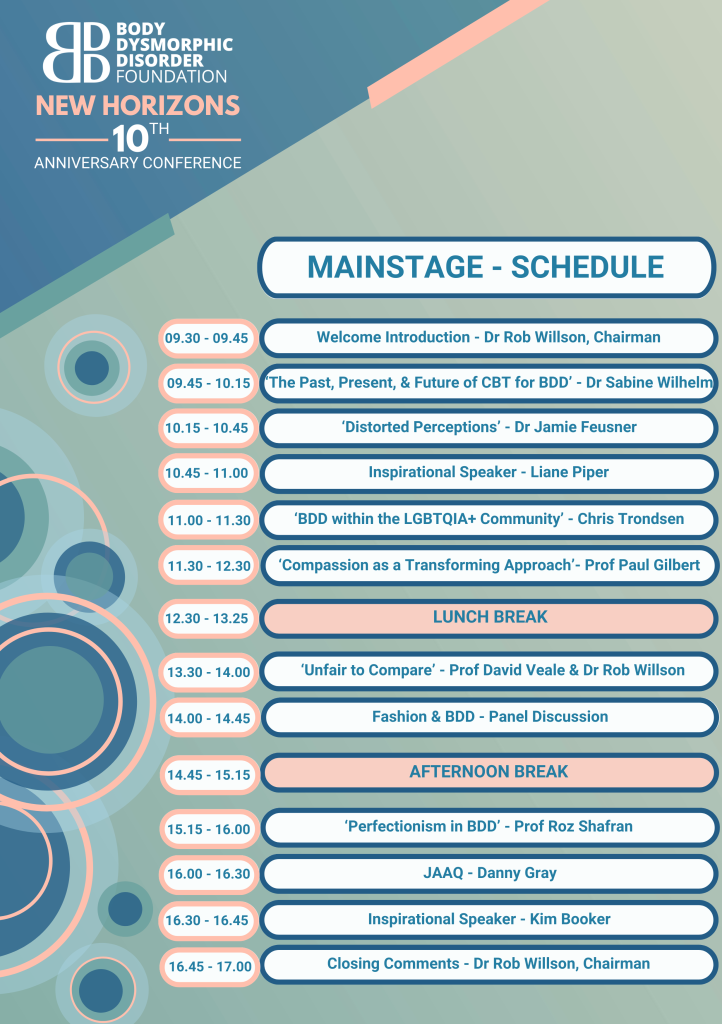



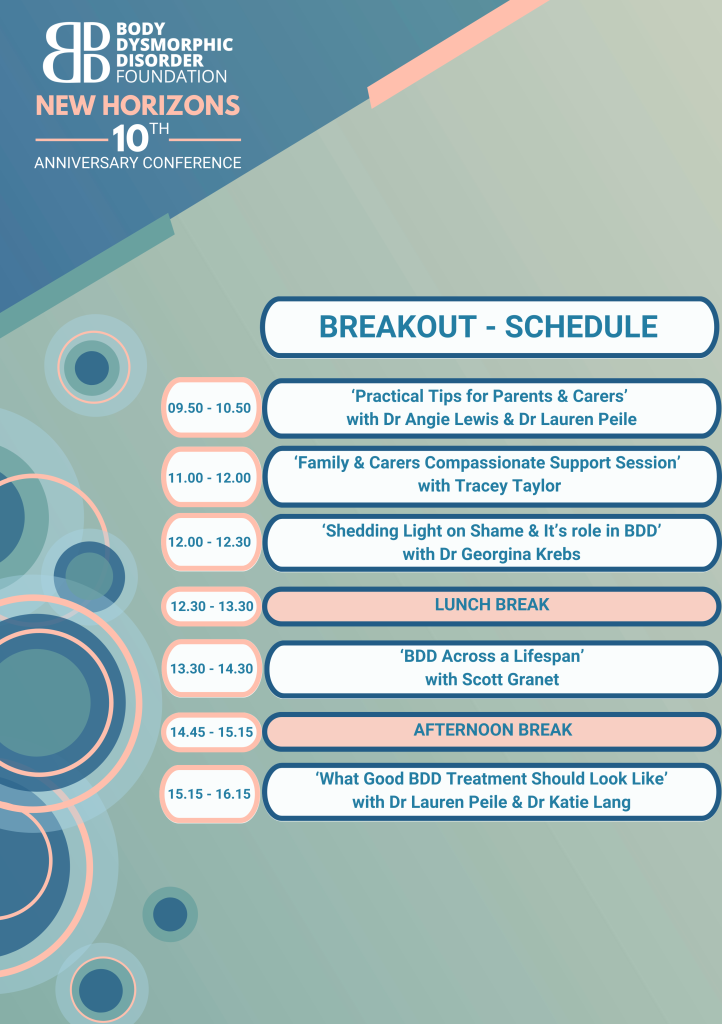

At this year’s conference, we are introducing a Support & Community Room, designed specifically for those who need a listening ear, are seeking community or just need some quiet time.
It will be a softly-lit, cosy and inclusive space for anyone who needs it. Our compassionate and understanding volunteers will welcome you into the space, where you can choose to take some time out, browse the BDD related artwork, sip on a cuppa, or have a chat with someone who truly understands the struggles of living with BDD. In addition to the artwork created by our wonderful community, there will also be a creative corner with resources to create something of your own or calm the mind.
We know how tough it can be for some individuals to attend the Conference and face so many people, so we hope this space provides some comfort and calm. It’s there for anyone who wants or needs to use it ![]()
Solidarity rate: for those who would otherwise be unable to attend for financial reasons or other barriers. We have a small number of bursary tickets available on a first come, first serve basis. Please contact info@bddfoundation.org for more details.
To avoid disappointment please consider purchasing your ticket to the physical conference early. In previous years we have sold out in advance.
No matter where you live you can now attend the conference via the internet with the option to attend via Webinar/Livestream for a reduced ticket price.
To reach as many people as possible, we will be filming the speakers on stage. Please be assured that the camera will be solely focused on the speakers and that all filming will be sensitively and discretely carried out. There will not be any recorded footage of attendees. If you have any concerns about this, please do not hesitate to approach one of our volunteers on the day.
All halls and rooms at 20 Bedford Way are accessible and a managed evacuation process is available from areas on levels 1 and 3 of the building for persons with mobility impairment. Logan Hall is situated on Level 1.
In previous years, we have gathered feedback from attendees, with many reflecting on the day as one which offers hope and connection. We aim for the day to be inspiring and informative to as many people as possible and hope this year’s event is of benefit to all. If there is anything we can do to support your attendance, or for any questions relating to the 2023 Conference, please email info@bddfoundation.org.
We look forward to seeing you in November for another successful event. It is a day not to be missed!
We are currently evaluating our services and working on our impact report, and we want to hear from you. We hope you will share your experiences of engaging with the BDD Foundation and the impact any of our services and our wider work has had on your life, or the lives of others.
We welcome responses from our entire community. This includes anyone with experience of BDD, including lived experience, providing support to someone experiencing BDD, carers, families, partners, friends, professionals and students.
If you prefer to send your thoughts through a different format or with a creative piece attached, please email impact@bddfoundation.org
Thank you for your input. As well as allowing us to measure our impact, your responses will contribute to the continued growth of the charity and allow us to stay user-led, and to identify our strengths, areas for development and most crucial services.
Survey closes: 11th October 2023
The feature on BDD shared the story of a BDD survivor and spoke with our trustee Dr Amita Jassi to understand more about the prevalence of BDD, how it might present, and the crucial need for further research and training on the condition in a clinical setting.
BBC News also highlighted Muscle Dysmorphia by speaking with our Chairman Dr Rob Willson and sufferer George Mycock. They discussed the severity of the condition, symptoms, and encourages those affected to access support. Muscle Dysmorphia is a serious, debilitating but treatable condition, with many of those suffering still not accessing the help and support they need.
Our support groups play an important role, alongside treatment, in recovering from and managing BDD. They provide a safe environment where people can talk openly about their BDD, as well as giving support and encouragement to others. Many attendees find comfort in shared experience, knowing they are not alone, and hearing stories from individuals at different stages of their recovery. More information can be found here.
For this role, it’s important to have a good understanding of BDD and the impact it has. We look for individuals with strong listening skills, an ability to make others feel welcome and comfortable, and empathy for others. We encourage applications from those with lived experience of BDD since these groups are peer led – an approach we have found to be particularly effective in supporting those experiencing BDD.
Training and induction will be provided. We require a minimum commitment of 1.5-3 hours per month.
“I found facilitating groups incredibly meaningful. Having suffered with BDD for most of my life and finding myself in a stable place of recovery, it felt really rewarding to support those who were at different stages of their journey with empathy and understanding.”
“I am confident that I learn as much from attendees as they do from me. Their honesty, insights, openness and support to one another is like nothing else, and I have had moments that bring up a lot of emotion because their experience resonates with me so much. I feel genuinely humbled and honoured to be a part of their BDD journey. It’s challenging at times, but incredibly rewarding.”
Download the Application Form below, and send completed applications to volunteers@bddfoundation.org
Applications will be reviewed and responded to by 18th August.
Researchers from the Centre for Addiction and Mental Health (CAMH) and the University of Toronto are looking for participants between the ages of 18 to 40 years who answered yes to any of the questions displayed on the poster, in addition to controls. Participants will be compensated for their time.
All participants must reside near and be able to travel to Toronto, Canada. The purpose of this visual processing study is to help us understand how individuals with BDD perceive themselves and how to best address their differences in visual processing.
If you fit these criteria and would like to participate in our study, please contact us at: bdd.empac@camh.ca

The Brain, Body, and Perception laboratory’s clinical neuroscience research seeks to understand the brain basis of perception, emotion, and reward across conditions involving body image as well as obsessions and compulsions. Additionally, they study gender identity, own body perception, and the effects of hormone treatments in individuals with gender dysphoria in the interest of improving health outcomes of gender-affirming treatments.
If you would like to learn more about the Brain, Body, and Perception laboratory and their research, visit: https://bbp.lab.utoronto.ca/ You can also learn more about the laboratory on Instagram (@bbplab) or Twitter (@BDD_anorexia).
At the end of June, the wonderful Michelle is embarking on a 46 mile walk to raise crucial funds for the BDD Foundation.
She will be completing Rotary Across Wales, walking across all of Wales in a day, from Machynlleth to Montgomery, in memory of her daughter Morgan-Rose.
The walk follows a mix of public rights of way, Glyndwr’s Way National Trail, country lanes and the meandering Montgomery Canal. Along the way passing through characterful communities and the settlements of Staylittle, Trefeglwys, Caersws, Newtown and Abermule.
It’s an admirable challenge and we are extremely grateful to Michelle for her fundraising efforts to the BDD Foundation.
For Ulrike’s master’s project at university, they have created a collection of six artworks focused on the theme of Body Dysmorphia. Ulrike would like to share their work with fellow sufferers to find out if their work resonates with you and receive some feedback.
Body dysmorphic disorder (BDD) is a body image problem that is marked by an intense preoccupation with one’s physical appearance. It can result in extensive gazing of one’s perceived flaws or – as in my case – in avoiding looking at oneself all together. For me, my body is an alien shell that carries me around and not something I can identify with. I cannot actually look at myself neither in the mirror nor in photos. The body of work created explores different approaches to visualise the tension between me and my body. Photographs were digitally manipulated, worked into and written upon. The object is the subject and vice versa. Initially connected by aversion, they show an attempt to be at peace.
Acceptance and Self Love (featured below) use my eyes perspective’s view of my body creating a neutral distance. It is not always possible to think positively during moments of struggle with BDD. Peace is found in admitting the negative thoughts.

Shadow Dance (featured below) confronts my body indirectly by its shadow, hereby creating enough distance and abstraction to allow looking at myself. Poses explore the interplay between the observer, the arranger, and the ‘me’. Twelve shadows are arranged as a group describing a story of curiosity, instability and peace.

The series Almost Within Reach (featured below) transport the idea of ‘making contact’ with a blurred image in the mirror. My hand is reaching out to the person on the other side offering peace. An impressionistic feel to it transfers the artwork to somewhere between dream and reality. Almost Within Reach III is covered with unfiltered thoughts about me, my art and my body. The text forms a veil and middle ground between the observer and the image. I am almost at peace with myself.

Thank you for taking the time to look at my artwork. Would you be willing to provide me with some feedback?
Does the work resonate with you?
What are thoughts going through your mind when seeing the images?
Would you say it conveys what a struggle with BDD can feel like?
Does the work highlight the frustration with the condition as well as giving a sense of hope?
Please connect with Ulrike to share your responses and feedback on ulrike.behrendt@student.nua.ac.uk